Header logo
header top contact widget
Implant Placement
Dental Implants – A Bionic Smile!
Posted on Sep 25, 2018 by William J. Claiborne, DDS MS
Modern medical science is amazing. Today’s technology has helped to advance the ability to provide miraculous solutions to many once-challenging problems. For example, “bionic” arms and hands have been developed to function almost normally. Today, prosthetic legs are moving people out of wheelchairs and into positions to walk and run.
When I think of dental implants, I realize just how miraculous they are as well. While some people think of dental implants as fairly recent on the scene, they have actually been around since the 1950’s. 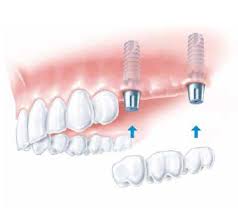
Like prosthetic limbs, many types of dental implants have been developed to accommodate specific needs. For example, one known as ‘All-On-4’ is designed for people who have lost a great deal of bone mass. Using a specific design and placement at unique angles, the All-On-Four system overcomes the problems of severe bone loss to support a full arch of non-removable teeth.
Other implant types can support one or a bridge of two or more replacement teeth. Some implant systems are ideal for placement at the time of tooth removal. Still, other systems work in conjunction with additional implants to support multiple teeth.
For individuals who have experienced bone loss (which commonly occurs from years of missing tooth roots), bone grafting can be performed prior to implant placement. Or, bone rebuilding materials can be added to existing bone to rebuild it.
Bone loss is a big deal, even though it’s not always obvious at first. Known as ‘resorption,’ this occurs when tooth roots no longer exist in the jaw bone that once supported natural teeth. Over time, the bone begins to shrink due to lack of stimulation.
Bone loss is the reason that once snug-fitting dentures begin to slip or move while eating. As the ‘ridge’ flattens (which is the gum-covered arch where tooth roots were once held), the foundation that the denture was originally made to conform declines in height. As the bone shrinks, the denture has less and less of a base to support it.
For people who are missing one or several natural teeth, it is paramount that they be replaced, preferably with dental implants. Why? Statistics show that natural teeth adjacent to a lost tooth are at greater risk for being the next to be lost.
Dental implants recreate stimulation to the jaw bone, thereby halting the pace of bone loss. When bone mass is maintained, neighboring teeth have a reduced risk for being lost as well.
Because dental implants are held in the jaw bone, they are also able to restore a natural biting strength with dependable stability. Having the ability to bite and chew efficiently and enjoy a diet of foods you love enhances eating pleasure and proper digestion. It’s no surprise that people who wear dentures have more gastrointestinal problems than those who have their natural teeth.
There are so many advantages to having dental implants. One of the best ones is their longevity. When dental implants are properly selected, placed and maintained, they should last your lifetime. This is why it’s so important to have your implant treatment through a Periodontist.
A periodontal specialist has advanced training and skills in the diagnosis and placement of all types of dental implants. He or she can enhance your ability to enjoy this miraculous tooth replacement option for your lifetime.
If you have lost natural teeth or are facing the potential of tooth removal, call 828-274-9440 to schedule a consultation. This will occur in a private, comfortable consultation room conveniently located in our Asheville office.
During this time, we’ll discuss the implant systems that may work best for your needs and preferences. I’ll explain the treatment involved and sedation options along with estimated treatment fees.
Just as you would want a hand or a leg replaced with a normal looking and functioning prosthetic, you certainly want replacement teeth that function properly and look as natural as the teeth you once had (or better!).
Call today and arrange an appointment to discuss getting your smile back to better-than-ever!
How A Denture Can Be Ruining Your Health
Posted on Aug 13, 2018 by William J. Claiborne, DDS MS
Since 1962, the U.S. has allowed pharmaceutical companies to advertise their drugs directly to the public. New Zealand is the only other country that has legalized this, which (to me) is rather telling of its ‘benefits’ in educating the general public.
It’s legality is not the issue here. In the promotions, these ads may name some of the side effects associated with that particular medication. These can include minor problems, such as “redness at the injection site,” to greater issues such as “weight gain,” to dire concerns, such as “increased risk for leukemia.”
Sometimes, it’s what you don’t know that can be the greatest detriment when it comes to our health and well-being. As a periodontal specialist, this has always been a particular concern: Do people really know the full story when it comes to dentures?
Since full dentures are not a prescribed medication, they are widely recommended and placed to replace a full ‘arch’ of upper or lower teeth. Although a denture can replace missing teeth, it falls very short when it comes to actually ‘restoring’ teeth.
There are far more things that a denture cannot do than what it can.
For example, a denture can give you the appearance of teeth and enable you to speak properly. A properly-fitted denture can also enable you to chew food again. But, the snug fit of a denture when initially made may be very different to how it fits a year later.
It is what occurs BENEATH the gums that can trigger a detrimental chain of events.
Natural tooth roots are held by the upper and lower jaw bones. With this as their foundation, tooth roots are able to support teeth that can function dependably. For example, having the sturdy foundation of the jaw bones, teeth can bite and chew with stability.
This means your teeth can endure the rigorous action of biting into a crunchy carrot or chewing a thick pork chop without the worry of movement. Natural teeth are held firmly by a solid mass of bone.
Here’s the problem many people are unaware exists: When the roots of natural teeth are removed from the jaw bone, the bone begins to shrink. This process is known as resorption. As the bone declines in height and width, the gum-covered ‘arch’ where teeth were once held begins to flatten out.
Because a denture is first made to conform to the specific contours of this arch, this means that the denture’s foundation is declining, providing less and less of a base for the denture to wrap.
Bone resorption is the beginning of a long list of problems.
When a denture is not secured by the bone, it must rely on what it rests upon. When the arch is high and full, the denture can hold on more securely while eating, speaking, or laughing.
However, as the arch shrinks, the added help of denture adhesives or pastes are needed. Unfortunately, once the denture begins to move or slip, the underlying problem will only worsen. As bone loss becomes more severe, these denture products will be of little help.
What a “rocky” denture does to your overall health often hides in the background. But, the problems exist all the same. For example, people find that eating some foods are too challenging for a denture. They resort to eating foods that are soft and dissolve easily in the mouth.

Wearing dentures can lead to alterations in food choices, often not-so-good ones.
A healthy diet includes foods that provide a balanced mix of protein, fiber, vitamins, and minerals. Plus, we want to eat foods that are flavorful and satisfying – right?!!! So, when a denture wearer switches from a kale salad to mashed potatoes, the trade-off is in nutrition along with the satisfaction that chewing provides.
There is an intricate relationship between the function of chewing and the brain’s ability to signal satiety (the perception of being full). When people are able to chew without the worry of a denture’s movement (which leads to uncomfortable rubbing on tender gum tissues), they are able to chew longer and more efficiently.
Additionally, proper chewing is a known support to the digestive process. In grade school, we all learned that the first phase of digestion begins in the mouth. As we chew, saliva automatically surges digestive acids into the mouth to help break down foods so they are ready to be processed further once swallowed.
However, not being able to chew well typically means it is done less. It is to no surprise that people who are denture wearers have more gastro-intestinal problems than people who have their own teeth. Of course, inadequate digestion causes a domino effect throughout the body.
In a 2013 article shared by the International Journal of Dentistry (through the U.S. National Library of Medicine/National Institutes of Health) edentulism (losing all of one’s natural teeth) leads to:
• Lower intake of fruits and vegetables, fiber, and carotene and increased cholesterol and saturated fats, in addition to a higher prevalence of obesity, increasing the risk of cardiovascular diseases and gastrointestinal disorders.
• higher rates of chronic inflammatory changes of the gastric lining, upper gastrointestinal and pancreatic cancer, and higher rates of peptic or duodenal ulcers.
• greater risk of noninsulin-dependent diabetes.
• greater risk of heart disease, hypertension, heart failure, and stroke.
• decreased daily function, physical activity, and resulting quality of life.
• higher risk of chronic kidney disease.
• higher risk of sleep apnea.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3664508/
The periodontal specialty includes the advanced training and skills of diagnosing and placing dental implants. They are so beneficial to your oral and overall health that this specialized branch of dentistry includes them in our ability to enhance the oral wellness of patients.
Dental implants are positioned in the jaw bone. This not only restores the same, sturdy foundation that natural teeth once had, the presence of the implanted portions provide stimulation to the bone.
Dental implants provide three major benefits…
(1). An implant helps to halt the process of bone loss, preserving bone mass. This not only supports the ability to bite and chew, dental implants enable eating to occur without movement. No more slips, clicks or uncomfortable rubbing on tender gums.
(2). With implants, people are able to eat a healthy diet AND chew it properly. This support digestion, which in turn supports every part of the body.
(3). When people feel confident smiling, laughing, and eating in social settings, they tend to be more active socially. Being active with other people is a basic human need and necessary for our mental well-being. When the fear of embarrassment because of “slippery” dentures is eliminated, people have more confidence in these settings.
If you wear dentures, PLEASE learn the facts surrounding dental implants. Many people assume they are too expensive. Yet, what is needed for your specific situation may be less expensive than you realize.
Often, just 4 or 6 strategically-placed implants can support a full arch of replacement teeth.
Too, many dental offices offer payment plans so monthly fees are manageable to most budgets. Some plans are interest-fee and require no down payment.
It is important, too, that you know this: Once bone loss begins, it will continue at a more rapid pace with each passing year. This means that your bone will become thinner and thinner at a faster and faster rate each year.
If you’re missing all of your natural teeth, call 828-274-9440 soon to schedule an implant consultation. During this time, I’ll explain the implant systems best for your needs and the process involved. I’ll also answer your questions thoroughly. This will help you make decisions that are right for you.
Gum Disease, Dental Implants – A Periodontist Can Make A BIG Difference.
Posted on Aug 06, 2018 by William J. Claiborne, DDS MS
When it comes to our health, most of us have an internist, or a ‘primary care’ physician. This doctor oversees our general health. However, should a strange rash appear, our internist will likely refer us to a dermatologist. The same is true if we experience persistent back pain; the internist is likely to refer us to an orthopedist.
When it comes to the best way to pinpoint and tackle specific issues with our health, it makes sense to see a doctor who has received specialized training in that area. This helps to take the guesswork out of diagnosis and enhances the potential for a successful outcome in an efficient process.
As a periodontal specialist, I work with a large number of general dentists in Western North Carolina as well as other dental specialists and physicians. In many cases, we work together in “team treatment” so the patient receives specialized dental care that blends comfortably with the positive relationship each has with his or her regular dentist.

Dr. William Claiborne,
Biltmore Periodontics
What is a periodontist?
A periodontist is a dentist who has continued in education to specialize in the diagnosis and treatment of all areas of the tissues in the mouth. In addition to treating all phases of periodontal (gum) disease, we are uniquely qualified to reshape gum tissues.
For gum disease, we are able to help patients overcome the problems caused by the infectious bacteria in the mouth. Through decades of research, this bacteria has been associated with many health problems elsewhere in the body. It has been found to trigger systemic inflammation and has been linked to a number of health problems, including heart disease, stroke, diabetes and arthritis.
We begin by accurately diagnosing the stage of gum disease present. From there, we develop a customized treatment plan based upon factors such as the patient’s current overall health, their diet, medications, whether they smoke or drink alcohol, and age.
Treatment recommendations are made based on what will effectively resolve the problem without over-treating or under-treating. By restoring the patient to good oral health, we are able to help them avoid tooth loss and rid their mouths (and thus, their bodies) from an overload of oral bacteria.
Gum tissues also play an important role in protecting teeth. When they recede, or pull away from the base of teeth, tooth roots may be exposed. These darker, sensitive areas can be re-covered through procedures that restore the protective seal around teeth as well as the level of the gum line, which plays an important role in a smile’s appearance.
A periodontist specializes in gum contouring to enhance the look of your smile. For example, when the gum tissues that arch over each tooth are a different levels, it can distract from a smile’s appearance. Through reshaping procedures (often referred to as a gingivectomy), we can correct this for a more balanced “smile line.”
The same is true for an individual who is born with a “gummy smile.” This occurs when too much gum tissue shows above top teeth in a full smile. Often, with minor reshaping or “crown lengthening” procedures, we can adjust the gums to a more esthetically-pleasing level.
Periodontists also specialize in the diagnosis and placement of dental implants. They are trained to understand all the intricate concepts involved in selecting the proper type of implant. Then, they are skilled at placing implants at proper depths and angles. As they oversee your “healing” time, periodontists are also able to optimize your comfort and outcome.
A periodontist receives 4 years of “undergraduate” training at a college or university and then goes on to earn a dental doctorate. After 4 years of dental school, they further their education for another 3-4 years before completing stringent requirements for a specialty certification in periodontics.
This 11 years of higher education is a commitment I made with enthusiasm, and I have relished staying on the cutting edge of new developments in the field throughout my career. On an ongoing basis, periodontal findings have revealed the integral connection between our oral health and our overall health.
As research continues, the understanding of good oral health as it benefits our overall health will hopefully become common knowledge to every individual. Sadly, our nation now has an adult population of nearly half that have some level of gum disease.
If you would benefits from the advanced skills of a periodontal specialist, please know that we are fully trained to attend to your specific periodontal needs in a comfortable, effective manner. Our entire team is committed to compassionate, respectful care that is appropriate for each need and our office is equipped to handle your care efficiently, effectively, and gently.
Call 828-274-9440 to learn more or to schedule a consultation.
Suffer From Rheumatoid Arthritis (RA)? Why To Make Good Oral Health A Priority.
Posted on Jul 23, 2018 by William J. Claiborne, DDS MS
Rheumatoid arthritis (RA) is a painful, debilitating disease. It is primarily known to destroy joints but can also affect internal organs (including heart, lungs, and kidneys). Although more common in older adults, RA can occur in younger ages as well, including adolescents and children.
For most people, the symptoms of RA begin with morning stiffness along with weak and aching muscles. As it worsens, joints become sore and stiff, most often affecting the fingers, wrists, elbows, hips, knees, ankles, toes, and neck.
An inflammatory disease, RA can further lead to swelling in the joints, disfigurement of the hands and feet, and numbness and tingling in the extremities. While there is no cure for RA, its discomfort and progression can be eased through medications, physical therapy, or surgery.
Like RA, periodontal (gum) disease is an inflammatory disease. And, like RA, gum disease causes pain, swelling, and tenderness. As it worsens, the inflammation can extend beyond the gums and attack the bone structures supporting the teeth as well as surrounding tissues. 
For years, research has been following the close connection between RA and gum disease. They’ve even noted that gum disease and RA share a genetic likeness, having similar pathogen structures ( agents that cause disease or illness). Another close similarity is in the formation process of both gum disease and RA.
And, the similarities between the two diseases continue further. While both conditions cause chronic inflammation in tissues that connect to bone, researchers have found the particular species of bacteria in each of nearly identical makeup.
A recent study has shown that people who are deemed “at risk” for RA have noteably higher incidences of gum disease. In the study, gum disease was diagnosed in 73 percent of individuals shown to have RA-associated antibodies before any evidence of joint disease (versus 38 percent of individuals without the antibody marker for RA). This suggests they originate from a site outside of the joints.
Perhaps from bacteria in the mouth? Based on its genetic similarities, this would be a logical conclusion.
The study, presented at the 2018 Annual European Congress of Rheumatology, took age, gender, and smoking into consideration. (http://www.dentistrytoday.com/news/industrynews/item/3499-gum-disease-may-initiate-autoimmunity-related-to-rheumatoid-arthritis)
Previous studies support this connection, even showing how a particular pathogen associated with periodontal disease activates the same destructive process of RA. On a positive note, research has shown that the successful treatment of gum disease can improve RA symptoms, which likely lessens the body’s inflammatory load.
A periodontal specialist has advanced training in the treatment of all stages of gum disease (as well as in the diagnosis and placement of dental implants). As a periodontist, it is troubling to know that nearly half of American adults have some level of gum disease. (https://www.perio.org/consumer/cdc-study.htm)
For our nation’s health, this poses a particular challenge since research continually reveals close connections between the bacteria of periodontal disease and serious health conditions. For example, research has linked gum disease to heart disease, stroke, memory loss, preterm babies, diabetes, some cancers (including pancreatic and lung cancer), Alzheimer’s disease, and impotency — in addition to its connections to RA.
I believe the prevalence of gum disease is mainly due to how its symptoms can go easily ignored until it’s potent bacteria are running rampant. By the time the disease is well underway, gum disease bacteria can have penetrated weakened gum tissues and entered the blood stream. This is how it is able to trigger inflammatory reactions that can reach far beyond the mouth.
When gum disease begins (due to an over-accumulation of oral bacteria), it causes the gums to become sore and often bleed when brushing. As the disease progresses, it can lead to persistent bad breath and gum tissues that darken in color. Untreated, pus pockets may form at the base of teeth and teeth can loosen. In advanced stages, teeth may require removal. Gum disease is the nation’s main reason for adult tooth loss.
The findings of research is indisputable in this: Our oral health is intricately connected to our overall health. As more adults understand how the presence of gum disease can greatly increase the risk for serious health conditions, we will hopefully see a better commitment to protect overall health through good oral health.
If you need to renew your own commitment to good oral health, or if you have signs of gum disease (as mentioned above), begin by calling 828-274-9440 to learn more or to schedule a consultation appointment (or tap here).
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012