Header logo
header top contact widget
Tooth Loss
Why Seek A Periodontist For Dental Implants
Posted on Jul 13, 2021 by William J. Claiborne, DDS MS
Like many people, I value my relationship with my Internist. Through his care, I am confident that he understands my specific needs to oversee all aspects of my health.
Some of this care occasionally involves being referred to a specialist. For example, my Internist may advise me to see a dermatologist for a particular skin condition. Together, my internist and the dermatologist are able to work in unison so I’m receiving the proper treatment plan according to my particular needs.
I am also a specialist in the dental field. I am a periodontist, which is a specialist who receives most patients through referrals by a general dentist or another dental specialist. This is because a periodontist offers a unique set of skills as well as an advanced level of understanding when it comes to oral tissues and dental implants.
The American Academy of Periodontology defines a Periodontist as: “A periodontist is a dentist who specializes in the prevention, diagnosis, and treatment of periodontal disease, and in the placement of dental implants. Periodontists are also experts in the treatment of oral inflammation. Periodontists receive extensive training in these areas, including three additional years of education beyond dental school. They are familiar with the latest techniques for diagnosing and treating periodontal disease, and are also trained in performing cosmetic periodontal procedures.”
(https://www.perio.org/consumer/what-is-a-periodontist)
To reach this specialty requires an individual to be highly committed. A periodontist begins education by completing 4 years of college (undergraduate training) and then continues another 4 years in dental school to earn a doctorate. To specialize in Periodontics, he or she must further their education for another 3-4 years before completing the stringent requirements for a specialty certification in periodontics.
In addition to treating all phases of periodontal (gum) disease, a periodontal specialist is uniquely qualified to reshape gum tissues. This may be performed to correct a “gummy smile” or even out a smile line through crown lengthening. Periodontists also specialize in the diagnosis and placement of dental implants.
The advantages of a periodontist in dental implant treatment are multi-faceted. This specialist is trained to understand the intricate concepts involved in selecting the proper type of implant and skilled at placing implants at proper depths and angles. A periodontist is also able to optimize patient comfort during treatment and throughout the healing phase.
Using his or her advanced training in the diagnosis and placement of dental implants, a periodontist can help you enjoy a higher potential for dental implant treatment that lasts a lifetime. There are a number of reasons you should strongly consider having a periodontal specialist involved in dental implant treatment, including:
SELECTION OF IMPLANTS – Dental implants come in a wide array of shapes and sizes. Each system is designed to accommodate certain needs and preferences. For example, some implants are designed to support a full arch of teeth while others can be placed in areas where a great deal of bone loss has occurred. The selection of the implant type that is appropriate for your needs and goals requires a unique understanding of all implant types. That is, a periodontist can select the type that will work best for you rather than go with the one or two in which they have received training.
PLACEMENT OF IMPLANTS – In addition to selecting the best type for your needs, proper placement of implants has a great deal to do with having a successful outcome. When an implant that is too long, for instance, is placed in bone that is too shallow, it can have future repercussions that may require its removal. This could occur when a lower implant is placed too close to a nerve that runs horizontal through the jaw bone (mandible). Or, when an upper implant is placed in shallow bone, it can work its way into the sinus cavity. A periodontal specialist considers intricate factors that can effect your potential for success.
STRUCTURAL ISSUES – In addition to the factors involved with bone loss, other issues can ‘make or break’ having a successful treatment outcome with dental implants. For example, for people who have bite misalignment or TMJ disorders, they may be grinding or clenching their teeth during sleep – often unknowingly. Telltale signs of ‘bruxing’ including remaining, natural teeth that are chipped or worn. These forces are enough to crack a walnut. When dental implants endure these forces, especially during their ‘healing’ phase, there is greater risk for implant failure. A periodontist considers these issues prior to your treatment, helping you to bypass problems that can result in eventual removal.
INDIVIDUALIZED TREATMENT CONSIDERATIONS – Our goal is to help you get the most from your dental implants. When there are individual habits or preferences that can complicate success, we work with each patient to help them enjoy their dental implants for a lifetime. For smokers, we advise ways to support saliva flow and minimize oral bacteria levels. For people who take certain medications that can interfere with oral moisture, we recommend methods to keep the mouth properly hydrated. And so on. We want to make sure your care is individualized so your potential for implant success is high!
OPTIMAL COMFORT – For added comfort and relaxation, we offer Oral sedation or I.V. sedation (twilight sleep) for most procedures for those who want or need these options. Both sedations are administered to the highest standards of safety possible. Our sedated patients are closely monitored throughout treatment with advanced safety equipment and trained professionals. Oral sedation is a pill that helps patients relax. It also has an amnesiac effect, leaving most with little or no memory of treatment afterward. I.V. sedation places the patient in a deeper sedative state, also erasing memory of the procedure. At our Asheville office, Biltmore Periodontics administers sedation with the involvement of a highly-trained doctor of anesthesiology for optimal comfort and safety.
For individuals who wish to replace one or more missing teeth, it makes sense that dental implants have become the leading preference. Dental implants restore the look, feel, and function like that of natural teeth. They also help to prevent bone shrinkage that occurs when tooth roots are no longer present in the jaw bone. This process is known as resorption.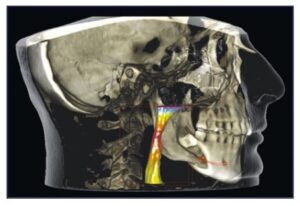
Resorption is what contributes to changes in facial appearance when the bone structures that give the face its shape start to shrink. When tooth roots no longer exist in the jaw bone, the stimulation once provided to the bone no longer exists. This causes the bone to shrink, or ‘resorb.’
As the bone mass declines in height and thins out, changes in facial appearance slowly evolve. For example, as the jaw bone thins, deep wrinkles form around the mouth. Eventually, the corners of the mouth will turn down even in a smile. Jowls form on each side of the face as facial muscles detach from the shrinking bone structure.
As the jaw bone continues to shrink, the chin becomes more pointed and the nose seems to get closer to it. This leads to a collapsed mouth that is known as a ‘granny look.’ This look ages the appearance of an individual far beyond their actual years.
Among the many benefits of dental implants, they also provide stimulation to the jaw bone. This helps to halt the process of bone loss. For those who have already lost a great deal of bone, bone rebuilding procedures can be performed to restore a healthy, more youthful face shape.
In addition to all the advantages of care through a periodontist, our Asheville periodontal office features some of the most advanced technology available. This includes laser dentistry and cone beam imaging as well as highly-advanced computerized options.
If you’ve considered dental implants to replace missing teeth, we invite you to consult with us during a private consultation appointment. A referral is not necessary. During this time, we will discuss your needs and goals as well as any concerns regarding comfort or costs.
To schedule, call (828) 274-9440.
Arthritis? Recommit Yourself To Having Good Oral Health.
Posted on Jun 20, 2021 by William J. Claiborne, DDS MS
According to the Centers For Disease Control & Prevention (CDC), over 47 percent of American adults are living with some level of gum disease. For those age 65 and older, this figure jumps to 70 percent.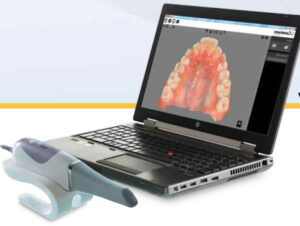
These concerning statistics are nothing to ignore. Although gum disease is so common, it increases risks that go far beyond the mouth. Over the years, research has tracked many diseases and conditions that correlate with gum disease bacteria. The inflammatory reactions triggered by these infectious bacteria have been linked to heart disease, stroke, some cancers, diabetes, preterm babies, and impotency.
Research has also shown a notably close relationship between gum disease and rheumatoid arthritis (RA). These studies have been ongoing for many years, and the findings should be concerning to all adults.
RA is a debilitating, painful disease that destroys joints. RA often emerges gradually, initially causing morning stiffness and weak, sore muscles. As inflammation from RA worsens, joints become swollen. Joints become achy and stiff most often in the fingers, wrists, elbows, hips, knees, ankles, toes and neck. Unfortunately, there is no cure for RA.
On a positive note, studies have shown that treating RA patients who have periodontal disease helps to improve RA symptoms. It is felt that this occurs because of a lighter burden of oral inflammation to the body’s immune system.
Below are some of the findings you may want to review. First, however, it’s important to understand how gum disease begins and some signs and symptoms.
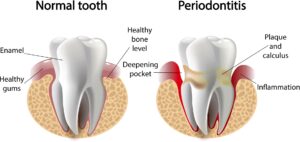
In the initial stage of periodontal (gum) disease, known as gingivitis, the gums may bleed when brushing. Bad breath is more frequent and the gums may be tender or swollen. As the disease progresses, the gums turn red and may pull away from the base of some teeth.
Bad breath becomes persistent and pus pockets may form at the base of some teeth. As the infectious bacteria attack the bone structures that support tooth roots, teeth will begin to loosen and may need removal. Gum disease is the leading cause of adult tooth loss in the U.S.
In addition to the devastating damage in the mouth, the infectious bacteria of gum disease can enter the bloodstream through diseased gum tissues, causing the inflammatory triggers that activate serious health problems, such as RA.
Years ago, researchers noticed an RA-perio trait among people with rheumatoid arthritis. While RA sufferers had gum disease more often, they observed that people with gum disease tended to have RA more often.
As researchers delved deeper into the connection, it appeared that the association is much more complicated than previously thought. Findings now suggest that oral bacteria could actually be a cause of rheumatoid arthritis.
In the past, doctors felt that periodontal disease was a result of RA itself since stiff, painful hands make it challenging to maintain good oral hygiene. They also suspected that medications prescribed to treat RA could be a factor since the drugs, which suppress the immune system, inhibited the body’s ability to fight harmful oral bacteria.
Both conditions cause chronic inflammation in tissues that connect to bone with both diseases having a similar inflammatory trigger. Even more similar is the particular species of bacteria found in periodontally-diseased tissues when compared with tissues around arthritic joints. In one study, a particular pathogen associated with periodontal disease was found to activate the same destructive process of rheumatoid arthritis.
In 2017, study findings were released by Johns Hopkins University Division of Rheumatology, which noted evidence that the tissues in the mouth of a periodontally-compromised individual and the tissues of the joint in RA have a number of likenesses. Research has also shown a genetic link between the two.
Above all, these findings reinforce how oral health correlates closely to our overall health. When you consider how the presence of gum disease can significantly increase your risk for serious health conditions, having good oral health should be a priority for every American.
What can you do to lower your risks for tooth loss and contributing to (or worsening) serious health problems? Recommit yourself to thorough oral hygiene at home and having twice-a-year exams and cleanings.
If you have signs of gum disease, have treatment at your earliest convenience. Gum disease will only worsen and requires more treatment time and expense as it progresses.
Call 828-274-9440 to schedule an examination, or begin with a consultation to discuss your needs.
https://www.hopkinsrheumatology.org/2017/01/gum-disease-linked-to-rheumatoid-arthritis/
https://www.cdc.gov/oralhealth/conditions/periodontal-disease.html
https://pubmed.ncbi.nlm.nih.gov/17551378/
Oral Bacteria Can Put An Immune System At A Disadvantage
Posted on May 20, 2021 by William J. Claiborne, DDS MS
Long before the COVID pandemic, it was widely known in the medical/dental and scientific communities that the bacteria in the mouth was intricately connected to the body’s overall health.
The oral cavity (interior of the mouth) contains some of the most varied and vast flora in the human body. It is the entryway for two systems vital to human function and physiology, the gastrointestinal and respiratory systems. Therefore, specific infections in the oral cavity may contribute to infection that can affect systemic health.
Systemic health refers to issues that affect the entire body, rather than a single organ or body part. An example of a systemic disorder is high blood pressure, which affects the body as a whole.
Research demonstrates that inflammation is a likely trigger for the systemic connection. For this reason, researchers have studied inflammation in the oral tissues caused by periodontal (gum) disease as a contributing factor of continual inflammation in the body.
 Hundreds of diseases and medications impact the oral cavity. Although the precise point of activation remains to be determined with some health problems, there is a more obvious association between oral bacteria and certain conditions.
Hundreds of diseases and medications impact the oral cavity. Although the precise point of activation remains to be determined with some health problems, there is a more obvious association between oral bacteria and certain conditions.
For instance, diabetes has a clear relationship with periodontal disease. Strong evidence shows that treating one condition positively impacts the other. By the same token, uncontrolled inflammation levels of one can worsen inflammation levels in the other.
Therefore, treating inflammation may not only help manage periodontal diseases but may also help manage other chronic inflammatory conditions.
Oral bacteria has been found to trigger or worsen other systemic conditions, including atherosclerotic vascular (heart) disease, pulmonary (respiratory) disease, diabetes, pregnancy-related complications, osteoporosis (bone loss), and kidney disease. A shared trait between gum disease and these medical conditions is that they are chronic conditions that take a long time to develop.
https://www.agd.org/docs/default-source/self-instruction-(gendent)/gendent_nd17_aafp_kane.pdf
According to the Centers of Disease Control & Prevention (CDC), nearly half of American adults ages 30 and over have gum disease – a whopping 47 percent. In a recent study, they found that about 9 percent have mild levels of gum disease, 30 percent have moderate levels and 8.5 percent have severe gum disease (periodontitis).
Researchers of a recent study found that 64 percent of adults ages 65 and older had either moderate or severe periodontitis. Gum disease rates were highest in males, Mexican Americans, adults with less than a high school education, adults below the poverty line and current smokers.
Although the initial stages of gum disease may be concealed behind the lips and cheeks, the interior of the mouth can signal the presence of periodontal disease at nearly every stage. For example, sore and swollen areas can indicate gingivitis, an early form of gum disease.
Worsening levels of gum disease can cause redness, tenderness, bad breath, bleeding when brushing, and receding gums. Progressive gum disease can lead to persistent bad breath, pus pockets forming around teeth, loosening teeth and painful chewing.
In your regular dental check-ups, your dental hygienist uses a “probe” to measure “pockets” along the base of teeth. During the exam, he or she measures the gum depth along each tooth – front, back and in-between. These depth measurements indicate areas where gum tissues have loosened from the base of teeth, and to what extent. The higher the number, the deeper the pocket.
 For example, healthy gums will measure 1 or 2. In some areas that are harder to reach when brushing or flossing, a 3 may be measured. However, a 4 or higher number indicates the gums are loosening their protective grip from the tooth. This leaves the tooth at risk for bacterial penetration below the gums.
For example, healthy gums will measure 1 or 2. In some areas that are harder to reach when brushing or flossing, a 3 may be measured. However, a 4 or higher number indicates the gums are loosening their protective grip from the tooth. This leaves the tooth at risk for bacterial penetration below the gums.
Healthy gums wrap snugly around the base of each tooth. This prevents the entry of bacteria, which can cause damage to the tissues and bone structures supporting tooth roots. Gum disease, to no surprise, is the nation’s leading cause of adult tooth loss.
However, infectious bacteria of gum disease don’t necessarily remain confined to the mouth. Through tears in diseased gum tissues, the bacteria are able to enter the bloodstream. Traveling through the body, these potent organisms can trigger reactions that activate or worsen serious health conditions.
For example, studies have indicated a relationship between periodontal disease and stroke. In one study focused on oral infection as a risk factor for stroke, people diagnosed with acute cerebrovascular ischemia showed a higher likelihood for having an oral infection than those who had healthy gums. (https://www.perio.org/consumer/gum-disease-and-heart-disease)
Along similar lines, men with gum disease have been found to be 49 percent more likely to develop kidney cancer, 54 percent more likely to develop pancreatic cancer, and 30 percent more likely to develop blood cancers.
Having healthy gums is actually easy – and rather inexpensive. Adults should brush thoroughly (at least 2 minutes) twice a day and floss daily. Snacking and sugar should be limited. The mouth should be kept moist throughout the day by drinking plenty of water (coffee, colas and tea doesn’t count). Moisture can also be replenished by the use of specially formulated oral rinses (available over-the-counter at many drug stores). By all means, drink alcohol moderately and avoid smoking.
Additionally, adults should maintain their 6-month dental check-ups and cleanings. These appointments help to remove any build-up of plaque or tartar on teeth so they are easier to maintain between visits. Too, your hygienist can point out areas of risk so you can concentrate appropriately during your at-home oral hygiene regimen.
If you’ve delayed (or avoided) regular dental care, your likelihood of having some level of gum disease is pretty high, even though you may not have obvious symptoms in early stages. Gum disease, once underway, does not go away on its own. It will gradually worsen and become a source of infectious bacteria that strains your immune system and increases your risks for serious health problems.
Begin with an examination appointment by calling our beautiful Asheville periodontal dental office at 828-274-9440. Here, we treat our patients with compassion, respect and with comfort a priority at all times. And, we provide patients with decades of experience and advanced skills — along with exceptional dental technology – so your treatment is successful and performed efficiently and effectively in minimal time.
While your smile is greatly important to your appearance, it’s what you can’t see that may harbor a rather ugly presence. Let’s get your smile in great shape!
Don’t Smoke? Living Or Working With A Smoker Creates Higher Risks Than Once Thought.
Posted on May 14, 2021 by William J. Claiborne, DDS MS
I doubt there is anyone in the U.S. who smokes tobacco who is unaware of the fact that it’s an unhealthy habit. Although the heart and lungs are more widely associated with the health risks of smoking, many people miss the fact that it is also damaging to the tissues in the mouth.
Consider the devastating statistics of COVID-19 related deaths in the U.S., nearing the 600,000 mark. Yet, when it comes to your oral health, cigarette smoking is responsible for more than 480,000 deaths per year in the United States. For people who don’t smoke but live or work with a smoker, secondhand smoke exposure accounts for over 41,000 of these.
For nonsmokers who are victims of secondhand smoke, that’s a tough statistic to accept.
Just how harmful is secondhand smoke? British researchers recently released some interesting findings along these lines. Their studies included several major countries and tracked nearly 7,000 adults, with nearly half being exposed to secondhand smoke. The findings showed that breathing in the smoke of another person’s cigarette can increase the risk of oral cancer by more than 50 percent. These cancers include lip, mouth and throat cancers.
On average, smokers die 10 years earlier than nonsmokers. For every person who dies because of smoking, at least 30 people live with a serious illness related to smoking. Smoking leads to disease and disability and harms nearly every organ of the body.
When considering the mouth, smoking can create costly problems in addition to a higher risk of tooth loss.
Twenty years of research shows that cigarette smoking is a risk factor for periodontitis. A smoker is 2 – 3 times as likely to develop periodontitis, which is an advanced stage of gum disease. In addition to increased prevalence, smokers also experience greater severity of gum disease.
Nicotine (in any form) has been shown to reduce blood flow in the gum tissues in the mouth. Pipe smoking can be worse than cigarettes due to the higher temperatures generated in the upper jaw. When it comes to dental implants, smoking is a risk factor for failure. It is also detrimental for conventional bridgework.
Cigarette smoking has long been associated with serious oral conditions, including periodontal (gum) disease, bone loss, tissue loss, and tooth loss. For smokers who opt for dental implants to replace missing teeth, they have a higher risk of peri-implantitis, which is inflammation of the soft and hard gum tissues surrounding a dental implant. To no surprise, smokers have a higher incidence of dental implant failure.
In an article published by the Journal of International’s Society of Preventive & Community Dentistry as far back as 2012, it warned that smoking can impact the rate of dental implant success, accounting for up to 20 percent of failures.
“Clinical trials of endosseous implants consistently rate smoking as a primary patient-centered risk factor for implant loss.”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894084/
It is common knowledge that the nicotine in cigarettes, e-cigs and ‘chew’ is an addictive drug. Some concerning quotes shared by the Oral Cancer Foundation are:
“Scientists have found that nicotine is as addictive as heroin, cocaine or amphetamines, and for most people, more addictive than alcohol,” states the article “Nicotine, Harder to Kick than Heroin,” published in the New York Times Magazine.
“Nicotine is similar in all critical measures to prototypic drugs of abuse such as cocaine, morphine and heroin.”
“Nicotine is a poison used as an insecticide.”
https://oralcancerfoundation.org/understanding/tobacco/tobacco-and-addiction/
Now, knowing the effects of secondhand smoke are likened to the non-smoking “victim” as inhaling half as many cigarettes as the user they live or work with, smokers should consider their habit in a different light.
While our Asheville periodontal dental office does not lecture or “guilt” our patients in any way, we feel they deserve to know the hazards of any risk factor related to the well being of their oral health. Without a doubt, smoking (whether cigarettes or vaping) is harmful to oral tissues and the potential to keep natural teeth.
In a report shared by Delta Dental, smokers are about twice as likely to lose their teeth than non-smokers, according to two 30-year studies at Tufts University in Boston. Their findings showed that men who smoke lose about 3 teeth for every 10 years of smoking, with women losing an average of 1.5 teeth per decade.
https://www.deltadentalins.com/oral_health/teethinpack.html
Every year, about half of smokers make some attempt at kicking the habit. Yet, only 6 or so percent are fully successful. All the while, the tobacco industry spends BILLIONS of dollars each year on cigarette and smokeless tobacco advertising and promotions.
According to the Centers for Disease Control & Prevention (CDC), in 2018 “$9.06 billion was spent on advertising and promotion of cigarettes and smokeless tobacco combined—about $25 million every day.” That’s more than $1 million dollars spent every hour of every day.
https://www.cdc.gov/tobacco/data_statistics/fact_sheets/economics/econ_facts/index.htm
While nicotine addiction means big money to the tobacco industry, it is enormously costly to our population. Now, knowing that secondhand smoke is so harmful to others, I hope our smoker patients will welcome our respectful support in their efforts to quit as we help them to maintain good oral health and keep their teeth (or dental implants) healthy for a lifetime of confident smiles.
If you’ve considered dental implants to replace missing teeth and smoke, please consult with us to discuss ways we can help you minimize the potential for dental implant failure. We want you to reap the benefits of a smile you’ll want to share proudly.
Call 828-274-9440 to schedule.
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012