Header logo
header top contact widget
dental specialist
Some Surprising Repercussions of Dental Fear
Posted on Mar 24, 2022 by William J. Claiborne, DDS MS
Dental fear has been ranked fifth among the most common of all fears, affecting nearly 50 million people in the U.S. Although a traumatic dental experience during childhood is often assumed to be the leading cause of dental fear, some findings show this is the case for about half of these adults.
For decades, dental fear has been to blame for many adults failing to have adequate oral health. Although cost, access, and awareness of need can be factors, nearly half of American adults avoid dentistry due to having some level of associated fear.
There are a number of false perceptions that don’t help lower this statistic. For example, a parent who tells a child “It won’t hurt much” before a dental visit simply sets the anticipation of pain into place. Hearing things like “That’ll be worse than a root canal,” and “nothing is wrong because nothing hurts,” add to the misconceptions when it comes to the reasons for avoiding regular, preventive dental care.
By some estimates, an adult with dental fear will endure pain for over two weeks to avoid seeing a dentist. They will self-medicate, use ice packs or try ‘home remedies’ found online, all to no avail. Some people end up in an emergency room because they could not force themselves to see a dentist.
Another factor may have to do with genetic makeup. In research conducted at the National Institute of Dental & Craniofacial Oral Health Research Center in Appalachia, “a gene variant was found that may contribute to heightened pain sensitivity and thus dental anxiety.”
https://www.proquest.com/openview/7df1b384b0fb8a79f854e9f304c524c1/1?pq-origsite=gscholar&cbl=30166
https://www.wiley.com/en-gb/Behavioral+Dentistry%2C+2nd+Edition-p-9781118272060
If you’ve ever heard the term, “you don’t know what you don’t know,” this is especially true for oral health. Although people are generally aware that insufficient oral hygiene can lead to bad breath and cavities, too many are unaware of some far worse consequences. Poor oral hygiene at home and lack of regular dental check-ups and cleanings form a straight line to developing periodontal (gum) disease.
While gum disease is the nation’s leading cause of adult tooth loss, it can also contribute to devastating health problems far beyond the mouth. The bacteria of gum disease are inflammatory. These infectious bacteria can enter the bloodstream through tears in weakened gum tissues, triggering a number of serious reactions.
To name a few, gum disease bacteria has been associated with the development or worsening of:
• Heart disease
• Stroke
• Alzheimer’s disease
• Pre-term babies
• Arthritis
• Diabetes
• High blood pressure
• Some cancers
Obviously, these bacteria are highly potent. Although being committed to a thorough, twice daily oral hygiene regimen at home is an important part of having good oral health, regular dental care is also necessary. These visits help to catch early signs of gum disease (which can begin without obvious symptoms). Early treatment can help to reduce treatment costs and time. And, the care can be essentially ‘painless’ when administered by the advanced skills of a periodontal specialist.
As a periodontist in Asheville NC, I want to be encouraging to adults about the risks associated with lack of dental care. I can cite the hazards of non-compliance of regular check-ups over and over. But, for people who have deep-seated fears when it comes to dental visits, far more support is needed to help an individual go from being fearful to relaxed.
A periodontal specialist has advanced training and skills in the diagnosis and placement of all types of dental implants. In our beautiful Asheville periodontal dental office, patient comfort is a priority at every visit. Our office is designed to pamper patients from the moment they enter. For certain procedures or patients who prefer the addition of sedatives, we offer oral sedation as well as I.V. sedation (twilight sleep).
Oral sedation is a pill that helps patients relax. It also has an amnesiac effect, leaving most with little or no memory of treatment afterward.
I.V. sedation places the patient in a deeper sleep state, also erasing memory of the procedure. It is administered by a doctor of anesthesiology for optimal comfort and safety. In our office, this is overseen by a board certified Anesthesiologist.
With both sedation options, patients are closely monitored with advanced safety equipment throughout treatment.
When patients realize our goal is to provide exceptional care in comfort, they relax. Over time, many patients feel they no longer need a sedative and are able to have regular dental care without worry.
Another way we enhance comfort for our patients is through our immense array of dental technology. In many cases, this advanced technology shortens both treatment time and speeds healing. For example, our LANAP (Laser-Assisted New Attachment Procedure) provides an advanced protocol to efficiently and effectively treat periodontitis (advanced gum disease).
Essentially non-surgical, LANAP treatment provides an alternative for patients with moderate to severe periodontal disease with a quick recovery time.
Regardless of numerous features to optimize patient comfort, it’s still difficult for many to feel ‘ready’ for dental care. We can reassure people on the phone, yet, some simply cannot make an appointment and actually arrive. This is why we often begin with a consultation in our comfortable, private consultation room. This room is removed from the clinical side of the office.
To learn more, call 828-274-9440 to begin with a consultation appointment. New patients are always welcome and a referral is not required.
Some Amazing History & ‘Back Stories” of Dental Implants!
Posted on Mar 11, 2022 by William J. Claiborne, DDS MS
Some “baby boomers” may recall a popular television show, The Six Million Dollar Man. The series ran from 1973 to 1978, with Lee Majors playing the role of Steve Austin, a former astronaut. After a NASA test flight accident, Steve had been rebuilt with bionic implants that gave him a number of superhuman qualities.
When this aired over 40 years ago, it seemed so futuristic; yet today, bionic implants are rather commonplace. One of the reasons is through the refined use of titanium.
Titanium was discovered in Great Britain in 1791 and named after the Titans of Greek mythology. Titanium is 60 percent denser than aluminum, but more than twice as strong. Titanium is non-magnetic, resistant to corrosion and has a strength-to-density ratio that is the highest of any metallic element.
Titanium can be alloyed (combined with additional element(s), such as iron, aluminum, vanadium, and other elements. These combinations can produce strong, lightweight alloys for a vast number of uses. Titanium is used for jet engines, missiles, spacecraft, and in the military, automotive, agriculture (farming) industries. Titanium is often used in medical prostheses, orthopedic implants, dental instruments used in root canals, and dental implants. Other uses range from components in sporting goods (such as golf clubs), jewelry and mobile phones.
Because titanium alloys have a high crack resistance, they are used in aircraft, armor plating, naval ships, spacecraft, and missiles. About two-thirds of all titanium metal produced is used in aircraft engines and frames. Titanium is also used in nuclear waste storage.
Because titanium is resistant to corrosion by sea water, it is used to make propeller shafts, rigging, and heat exchangers in desalination plants; along with many other uses for salt water components. Titanium is used in the housings and components of ocean-deployed surveillance and monitoring devices for science and the military.
The human body has also been given the advantages of titanium as it is biocompatible (non-toxic and not rejected by the body). Titanium is often used in surgical instruments, such as those used in image-guided surgery, as well as wheelchairs, crutches, and any other products where high strength and low weight are desirable. Inside the body, titanium is common in surgical implements and implants, such as hip balls and sockets (joint replacement) and dental implants that can remain dependably positioned for decades.
For orthopedic implants, the use of titanium means that skeletal loads are more evenly shared between bone and implant. This lowers the potential for bone degradation due to stress, reducing the risk of bone fractures, which have a tendency to occur at the boundaries of orthopedic implants.
Patients with titanium implants can be safely examined with magnetic resonance imaging (MRI).
When you think of dental implants – or other implants-in-bone, such as knees, hip joints, etc. – titanium has the remarkable ability to osseointegrate. Osseointegration is a term used when an artificial implant is surgically anchored into bone, in which the bone then grows around the implant. This restores strength and stability to the bone that can offer a lifetime solution.
The bone in which an implant is placed also benefits from the presence of titanium. In the jaw bone, where natural tooth roots are missing, their absence leaves the bone mass without stimulation once provided by the tooth’s roots. This stimulation is what helps the bone to maintain its mass.
Once bone loss begins, the pace of bone shrinkage, known as resorption, accelerates over time. The declining bone mass soon begins to cause a number of problems, including a change in the way a denture or partial fits.
Additionally, losing jaw bone mass causes changes in facial appearance. It may first appear as deep wrinkling around the mouth and as the corners of the mouth begin to turn downward, even when smiling. Jowls form as facial muscles detach from the shrinking bone. Over time, the mouth begins to sink inward and the chin moves closer to the tip of the nose.
Placing a dental implant into the bone halts the process of resorption. It recreates the stimulation once provided by natural tooth roots. And, because of the strength and stability of the implanted portions, patients with dental implants can rely on eating the foods they love again, biting and chewing with confidence.
https://en.wikipedia.org/wiki/Titanium
Having teeth is important for a number of reasons (eating, speech, appearance), which has been recognized throughout history. The first evidence of dental implants is attributed to the Mayan population roughly around 600 AD where they excelled in utilizing pieces of shells as implants as a replacement for mandibular teeth. Radiographs of Mayan mandibles show compact bone formation around the implants. It has also been found that, around 800 AD, a stone implant was shaped and placed in the lower jaw in early Honduran culture.
In addition to being the first U.S. president, George Washington is famous for his “wooden” teeth. History reveals that Mr. Washington suffered from dental problems from his twenties on. As a matter of fact, in his First Inaugural Address speech in 1789, Washington had only a single remaining natural tooth. Over the years, he wore several sets of dentures, but none made of wood. These were fashioned out of materials that included ivory, gold, lead, and human teeth.
In a letter to Washington from dentist John Greenwood (who fabricated dentures for Washington), he pointed out the staining of the dentures, likely due to consumption of Port wine. Dr. Greenwood cited the staining was what gave the dentures a grained, wooden appearance.
https://www.mountvernon.org/library/digitalhistory/digital-encyclopedia/article/wooden-teeth-myth/
Today, most of the “teeth” portions (restorations) are made of porcelain. Porcelain provides the most natural look and feel of “real” teeth with a similar luminosity of that of natural teeth. Porcelain is also highly durable the most resistant to staining.
To clarify a “dental implant”, it is a term that sums up what is actually a combination of components. Dental implants are typically three segments – the implanted portion that is held in the jaw bone, a post (abutment) that is positioned inside the implant and extends above the gums, and the attached replacement teeth (restorations).
A periodontist has have three years of specialized training beyond dental school to make them experts on both soft and hard tissues. Thus, they have the ideal combination of experience and knowledge to make sure you get a dental implant solution that looks and feels like your own teeth.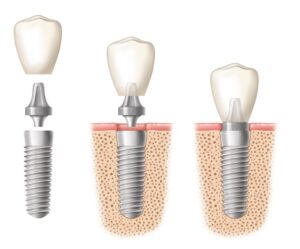
Because many people have lost one or more teeth due to periodontal disease, periodontists are an ideal choice in helping restore the gums to a healthy state while determining the best type of dental implant, and then placing the implant at the proper angle and depth.
Additionally, a periodontist can perform pre-implant placement procedures, which may be needed in certain cases. These can include:
Sinus Augmentation – The upper back jaw has traditionally been one of the most difficult areas to successfully place dental implants due to insufficient bone quantity and quality and the close proximity to the sinus. Sinus augmentation can help correct this problem by raising the sinus floor and developing bone for the placement of dental implants.
Ridge Modification – Deformities in the upper or lower jaw can leave you with and inadequate amount of bone in which to place dental implants. To correct the problem, the gum is lifted away from the ridge to expose the void where bone is missing. The void is then filled with bone or bone substitute to build up the ridge. Ridge modification has been shown to greatly improve the jaw’s appearance and increase the chances of successful implants.
Once your dental implant(s) is in place, your periodontal specialist can create a plan to help you maintain healthy implants, particularly in the prevention of peri-implant disease.
Peri-implant diseases are inflammatory conditions affecting the soft and hard gum tissues around dental implants. Similar to a natural tooth, bacteria can build up on the base of the implant, below the gum line. Over time, the bacteria irritate the gum tissue, causing it to become inflamed, damaging the tissue and if not caught early, causing the bone structure below the implant to deteriorate.
The history of dental implants is interesting, yet, what people want is to have their smile back and to enjoy the function of “real” teeth. Although the back stories of dental implants are many, what is most important is that we restore your smile and help you enjoy it for your lifetime.
Begin with a consultation in our comfortable Asheville periodontal dental office. Here, we can discuss what may be best for your needs in a private setting. We can discuss comfort options (including sedation), and estimated costs and treatment time. Here, you will be respected and treated with the compassion we would want for ourselves and loved ones.
Call 828-274-9440 to begin. You’ll speak with a member of our staff who will be happy to assist you.
ED Risks Higher With Presence of Gum Disease
Posted on Feb 25, 2022 by William J. Claiborne, DDS MS
For over two decades, medical researchers have closely focused on inflammation in the body and its power to activate health problems, heart and cardiovascular diseases in particular.
It has been determined that inflammation anywhere in the body can set off a series of biochemical changes in the bloodstream; those that are designed to help the body repair inflamed tissues. However, when inflammation becomes chronic, blood chemistry never returns to normal, and trouble ensues. Researchers have noted this significantly in its increased risk of heart attack and stroke.

Think of chronic inflammation as a pan of water that is boiling on the stove. When the body is in proper control, the boiling process ceases when the stove is turned to “off.” In chronic inflammation, however, the water continues to boil even after the pan is removed from the stove top.
Chronic inflammation can exist in the mouth, set at a constant “boiling point” due to advanced gum disease (known as periodontitis). Common symptoms are puffy gums that turn red in color; inflamed, swollen, or bleeding gums; gums that loosen from the base of teeth; persistent bad breath; gums that become spongy and bleed easily; and, pus pockets that form on the gums at the base of teeth.
In addition to creating higher risks of heart disease and stroke, advanced gum disease has been shown to increase the risks for diabetes, arthritis, preterm babies, some cancers, Alzheimer’s disease, high blood pressure and erectile dysfunction (ED). Yes, even ED.
Below are findings of several recent studies showing that periodontitis to be a significant risk factor for erectile dysfunction. Rather telling is as gum disease worsens, so does erection impairment.
• Turkish investigators studied 162 men, age 30 to 40. Eighty-two of the participants had normal erection function and 80 who complained of ED. Some men in both groups had chronic periodontitis, but the condition was more than twice as prevalent in the ED group. Men with periodontitis who also presented with decayed or missing teeth showed the greatest level of ED.
• Chinese scientists examined data of several studies involving a total of 213,076 men. Compared with those who had good erection function, those with ED had three times the risk of periodontal disease.
• The University of Granada School of Dentistry found that men with severe gum disease are more than twice as likely to suffer from erectile dysfunction. This was true even after careful adjustments were made for other health issues that could distort the findings, including socioeconomic data. In the study, 80 men with clear indications of erectile dysfunction were given a periodontal examination. According to the researchers, 74 percent of the participants with ED also presented with chronic periodontitis. The researchers concluded that patients with chronic periodontitis were more likely to have erectile dysfunction independent of other confounders.
• Israeli researchers surveyed the erection function of 305 men, average age 40, and then examined their gums. Those with chronic periodontitis had the greatest risk of ED.
The connection is actually logical. Periodontal disease has emerged as an independent risk factor for cardiovascular disease, and cardiovascular disease raises risk for ED. These studies show that everything that raises the risk for cardiovascular disease (such as smoking, obesity, chronic stress, high cholesterol, high blood pressure, and chronic sleep apnea) also raises the risk of ED.
This finding also makes biochemical sense. During sexual arousal, the body releases nitric oxide, which plays a key role in enabling erection. Chronic inflammations, including periodontal disease, impairs release of nitric oxide and contributes to ED.
Health risks such as our propensity for cancer or a decline in eyesight can occur regardless of lifestyle choices. However, it makes perfect sense to eliminate or greatly minimize risk factors, including periodontal disease. Research findings on ED’s association with infectious oral bacteria of gum disease will hopefully spurn more men to devote a higher level of commitment to care for their gums.
It takes mere minutes a day to maintain a healthy mouth and reduce the risks for developing gum disease.
 These include brushing teeth for at least two minutes twice a day. Daily flossing will remove bacteria in the gums that may elude brushing. And, keeping the mouth moist will support saliva flow, the mouth’s natural rinsing agent.
These include brushing teeth for at least two minutes twice a day. Daily flossing will remove bacteria in the gums that may elude brushing. And, keeping the mouth moist will support saliva flow, the mouth’s natural rinsing agent.
If you feel your erections are worth the effort, then these measures will become higher priorities in your daily hygiene upkeep. It is also important to see a dentist regularly. If you don’t feel anything is wrong because “nothing hurts,” you are only cheating yourself.
Gum disease can exist without obvious symptoms. Catching it early and before it begins to “boil” will help you avoid costly and time-consuming treatment later. And, these steps may keep your sex life active.
If you are experiencing any of the signs of gum disease (as mentioned prior), please know that gum disease will only worsen without treatment. It is also the leading cause of adult tooth loss.
A periodontist is a dental specialist who treats all stages of gum disease. If it is found to exist, this periodontal specialist can help to resolve the problem and restore your smile to a healthy state in the most conservative way possible. He or she can then help you maintain good oral health, which will support your overall health.
For an examination, or to begin with a consultation, call 828-274-9440.
https://onlinelibrary.wiley.com/doi/abs/10.1111/jcpe.12909?af=R
HPV – How The Virus Relates To Oral & Throat Cancers
Posted on Feb 17, 2022 by William J. Claiborne, DDS MS
Every April, a number of oral health and cancer organizations come together to recognize Oral Cancer Awareness Month on a national basis. This is meant to expand awareness of this cancer, which takes a victim every hour of every day. Of those individuals, 43 percent will not survive longer than five years. Those who do survive may suffer from problems, such as severe facial disfigurement or difficulties with eating and speaking.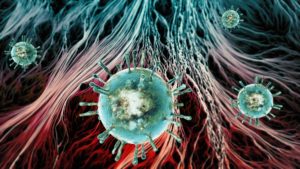
Oral cancer includes cancer of the mouth and upper throat, known as oropharyngeal cancer. The death rate associated with oral and oropharyngeal cancers is particularly high largely because detection typically occurs late in its development. However, when oral cancer is detected and treated early, treatment-related problems are reduced and with improved survival rates.
Annual oral cancer examinations during regular dental check-ups are the best method for detecting oral cancer in its early stages. It is also important to respond immediately to signs and symptoms of oral cancer, which include:
• A sore or ulceration that does not heal within 14 days;
• A red, white, or black discoloration of the soft tissues of the mouth;
• An abnormality that bleeds easily;
• A lump or hard spot in the tissue, usually border of the tongue;
• Raised tissue or a newly emerged growth;
• A sore beneath a denture or partial that does not heal;
• A lump or thickening that develops in the mouth; and
• A painless, firm, fixated lump on the outside of the neck that does not go away within two weeks.
Historically, factors that can contribute to having a higher risk of oral and oropharyngeal cancers have been heavy drinkers and smokers older than age 50. However, in recent years the cancer is occurring more often in nonsmoking people due to HPV 16, the virus most commonly associated with cervical cancer.
The human papilloma virus 16 (HPV) is sexually transmitted, although it is a different virus than HIV or (HSV) herpes. HPV is now the most common sexually transmitted infection (STI) in the United States.
Exposure can occur by having vaginal, anal, or oral sex with someone who has the virus. It most commonly spreads during anal or vaginal sex. It can also spread through close skin-to-skin touching during sex. HPV can spread even when a person with the infection has no signs or symptoms.
There are many different types of HPV; most do not cause any health problems. Most individuals who get HPV never have symptoms and the virus goes away by itself. But, if HPV does not go away, it can cause genital warts or certain kinds of cancer. Symptoms can appear years after having sex with someone who has the infection.
Approximately 99 percent of people who develop HPV will clear the virus on their own. In approximately 1 percent of individuals, the immune system will not clear the virus and it can lay dormant for decades before potentially causing a cancer.
HPV itself isn’t a cancer but it can cause changes in the body that lead to cancer. Because of the growing rate of HPV, the increasing incidence of oropharyngeal cancer have been particularly concerning for younger age groups. Within the age range of 15 to 59, 40 percent will have HPV. This is an alarming rate for people with no other risk factors.
HPV-related oral cancer most commonly involves lymphoid tissue in the tonsils or the base of the tongue. Signs and symptoms of HPV-caused oropharyngeal cancer may include one or more of the following:
• Hoarseness or sore throat that does not resolve within a few weeks;
• A swollen tonsil on one side (usually painless);
• A painless, firm, fixated lump felt on the outside of the neck, which has been present for two weeks or more;
• A persistent cough that does not resolve after many days;
• Difficulty swallowing or feeling something is caught in your throat; and/or
• An earache on one side that persists for more than a few days.
https://oralcancerfoundation.org/april-is-oral-cancer-awareness-month-2021/
https://www.cdc.gov/std/hpv/stdfact-hpv-and-men.htm
Cervical cancer is the most common HPV-associated cancer among women (48 percent), and oropharyngeal cancers (82 percent) are the most common among men. The diagnosis may not be until years, or even decades, after a person gets HPV. Currently, there is no way to know who will get cancer after getting HPV.
https://www.cdc.gov/cancer/uscs/about/data-briefs/no26-hpv-assoc-cancers-UnitedStates-2014-2018.htm
HPV vaccines can prevent some of the health effects HPV causes. Once acquired, however, there is no specific treatment for HPV although there are treatments for health problems that develop from HPV, such as genital warts. Your healthcare provider can treat genital warts with prescription medication.
Because cancers from HPV are more treatable when found and treated early, it is important for those who acquire the virus to be especially diligent in having oral cancer screenings and promptly responding to any signs or symptoms (as mentioned above).
The HPV vaccine is safe and shown to be effective at preventing the virus. Like any vaccine, side effects can occur, which are typically short-lived and mild, such as headache, fatigue, fever or nausea. Most people have no side effects at all.
You are also urged to be committed to your 6-month dental exams. This provides your dentist an opportunity to note any suspicious areas in the mouth or on the lips. If you have not had regular dental check-ups, you may need to begin by seeing a periodontal specialist.
A periodontist is a dentist who specializes in the prevention, diagnosis, and treatment of periodontal disease (a chronic inflammatory disease that affects the gums and bone supporting the teeth also known as gum disease), and in the placement of dental implants. Periodontists receive extensive training in both of these areas and more, including three additional years of education beyond dental school.
As a periodontal specialist in Asheville for over 25 years, I take great pride in making our patients feel comfortable and understanding of their particular oral health status. If oral problems exist, we are able to resolve many with conservative treatment measures. Our Western NC periodontal dental office features some of the most advanced technology available to minimize treatment needs, treatment time, and speed healing with comfort always a priority. Oral and IV sedation are available.
To schedule an appointment, call 828-274-9440. New patients are always welcome and a referral is not required.
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012