Header logo
header top contact widget
Oral Cancer
Read Label Before Purchasing Mouthwash
Posted on May 08, 2015 by William J. Claiborne, DDS MS
Mouthwash is a common component of many oral hygiene routines at home. For many patients, we recommend certain mouthwashes for their ability to kill oral bacteria, add fluoride, and treat particular mouth sores. Too, some mouthwashes are advised following extraction of teeth to curtail bacteria in areas where brushing must be postponed.
While many people assume mouthwash is a beneficial addition to brushing and flossing, not all are recommended by our office. Some mouthwashes contain alcohol, which dries out oral tissues. Even though alcohol kills oral bacteria, it also serves as a drying agent. This actually increases your risk for cavities and bad breath since alcohol decreases saliva flow.
Saliva is the mouth’s natural cleanser, keeping oral tissues moist and moving bacteria (and food particles that cause bacterial growth) out of the mouth. Some medications, smoking and drinking alcoholic beverages can also lead to dry mouth.
Additionally, it is suspected that regular use of mouthwash containing alcohol can lead to dental erosion.
Mouthwashes that contain alcohol have also come under fire for increasing the risk of oral cancer. Although these findings are still in research stages, it is suspected that alcohol becomes a carcinogen in the mouth, which is a cancer causing agent. Researchers have found that oral cancer risk is five times higher for those using alcohol-containing mouthwashes, even if they are non-smokers.
Like any product, always read the label of mouthwash before purchasing. Look for alcohol-free types and those with fluoride additives. Use after brushing and flossing and practice a gargling action to get the mouthwash to the back of your mouth. Since the back of your tongue harbors more oral bacteria than the front, consider using a tongue scraper prior to mouthwash. This loosens oral bacteria that are embedded in the tongue’s surface. You can also brush your tongue with your toothbrush following teeth brushing.
Remember, any mouthwash use is an addition to brushing and flossing, never as a replacement. However, certain mouthwashes can help keep your breath fresher, decrease your risk for cavities and support your oral health overall. Swish away!
Mouth Sore? Could Be A Canker Sore.
Posted on Apr 26, 2015 by William J. Claiborne, DDS MS
Because of the devastating statistics associated with oral cancer, any sore or unusual spot in the mouth should be monitored carefully. However, some sores that occur inside the mouth can be canker sores.
A canker sore is a painful spot that appears on the tongue, inside of cheek or on the soft palate. Canker sores are white or gray circles with a red outline. They may begin with a tingling or burning sensation before the sore appears.
While stress or tissue injury is often suspected to be the reason canker sores arise, their exact cause is actually unknown. Tissue damage can occur from things like wearing braces, biting the inside of the cheek or a tooth that cuts into tender oral tissue. Citrus or acidic fruits and vegetables can also be a possible cause of canker sores.
Canker sores may also be caused by a compromised immune system, B vitamin or iron deficiency, or diseases such as Crohn’s disease or celiac disease.
Fortunately, a canker sore doesn’t last long with discomfort subsiding in just a few days. They typically heal completely in less than two weeks. To speed healing, a prescription mouth rinse or ointment can be provided. Discomfort can also be lessened by some over-the-counter medications.
For people who have reoccurring canker sores, they should avoid citrus, spicy or acidic foods. Using a soft-bristled tooth brush is also advised.
A Periodontist specializes in treating gum tissues and should be contacted when canker sores seem unusually large, are multiplying or last longer than two weeks. Also, see a Periodontist when canker sore pain becomes extreme or is accompanied by a high fever. Call (828) 274-9440 for prompt attention.
Are YOU At Risk For Oral Cancer?
Posted on Apr 08, 2015 by William J. Claiborne, DDS MS
None of us anticipate contracting cancer in our lifetime. We may have a family history of certain cancers or know we’re risking cancer from certain lifestyle choices, such as smoking. Yet, the actual diagnosis of cancer is typically an unexpected jolt.
Oral cancer fails to be as visible as some other cancers, such as breast or colon cancer. It doesn’t have the backing of major media campaigns nor is it backed by nationally-coordinated fundraisers, such as walks sponsored by major firms. Yet, oral cancer is one of the deadliest of all cancers with one of the poorest survival rates. For those who do survive, the disfiguring effects from treatment can be jarring. Roger Ebert, one of the most recognized movie critics of modern film, succumbed to oral cancer after undergoing surgical attempts to save him, leaving him unrecognizable in his final days.
The American Cancer Society cites oral cancer is more than twice as common in men as in women. It is about equally common in blacks and in whites. Although the overall rate of new cases has been stable in men and decreasing slightly in women, there has been an increase in cases linked to infection with human papilloma virus (HPV) in white males and females.
Oral cancer occurs most often in:
• The tongue
• The tonsils & oropharynx
• The gums, base of the mouth and in other oral soft tissues
• The lips and salivary glands
The average age of people diagnosed with these cancers is 62 with more than a fourth of oral cancers occurring in patients under age 55.
With newly diagnosed oral cancer patients, a small percentage will develop another cancer in a nearby area such as the larynx (voice box), the esophagus (the tube in the throat) or the lung. Some who are cured of oral cancer will develop another cancer later in the lung, mouth, throat, or other nearby areas. For this reason, patients must have follow-up exams for the rest of their lives. Oral cancer survivors must also avoid tobacco and alcohol, which increase the risk for these second cancers.
The word “cancer” on its own is scary. For those who must endure the battle as well as family members who are closely involved, an oral cancer diagnosis is devastating. But, it doesn’t have to be a death sentence. Knowing your risks can help, but watching for signs and taking immediate action can mean the difference between minimal treatment versus a disfiguring, or even deadly, outcome.
Warning signs include a mouth sore that does not heal, white or red patch of tissue, difficulty swallowing, a lump or mass in the mouth or neck, a long period of hoarseness, pain or numbness in the oral region, change in the voice, or a long period of ear pain.
As a Periodontal Specialist, I have in-depth training that helps me spot early signs of oral cancer and to begin prompt treatment. My goal is to help restore you to good oral health in all procedures. Catching oral cancer as early as possible will help you resume your life with a smile.
If you have signs of oral cancer, as listed above, contact us immediately for an examination: (828) 274-9440.
Why Your Jaw Bone Is Shrinking
Posted on Feb 04, 2015 by William J. Claiborne, DDS MS
Natural teeth are held into your jawbones by their tooth roots, which are embedded in the bone. Throughout the day, actions such as biting and chewing create physical stimulation to the jaw by each root. The tooth roots stimulate the bone so it maintains a healthy mass.
Once natural teeth are removed, the lower and upper jaw bone structures begin to shrink (or ‘resorb’) due to the lack of stimulation. While conditions such as osteoporosis, gum disease and oral cancer can attack healthy bone structure, the leading cause of bone loss (‘resorption’) is missing tooth roots.
Although dentures and partial dentures provide low cost replacement of teeth, they actually accelerate this rate of bone loss. These rest on top of gum tissue, placing pressure on the jaw bone ridge whiling providing no direct stimulation to the bone.
Custom bridges, a popular treatment for replacing missing teeth, are no help, either. The bone underlying the span of missing teeth will experience resorption since no bone stimulation is provided.
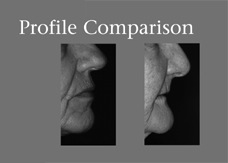
There are many repercussions to bone resorption. Facial changes can be seen at early stages by removing dentures or partials and looking in the mirror. Once bone loss is underway, you’ll notice your mouth seems to collapse into the face, the chin becomes more pointed, and deep wrinkles form around the mouth. Eventually, jowls form from the detachment of facial muscles from the jaws.
This photo shows a healthy bone mass compared to a resorbed jaw bone from tooth loss.
Other signs of bone loss are: Periodic changes in the way your denture fits; Sore spots on gum tissues; Food becoming trapped between the gums and denture; and, Difficulty chewing even with the help of denture adhesives and pastes.
Because they are secured by the jaw bone, Dental Implants recreate the stimulation of the natural tooth roots you once had. This halts the rate of bone loss and preserves bone mass. For those who have already experienced severe bone loss, bone rebuilding procedures can be performed to restore adequate bone structure.
Let’s discuss a confident, secure and dependable smile during a consultation appointment. Call (828) 274-9440 to schedule.
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012