Header logo
header top contact widget
Sore or swollen gums
Rocky Dentures? Why Relines Are Of Little Help.
Posted on Mar 16, 2016 by William J. Claiborne, DDS MS
As a dental specialist, I am referred most of our patients by other dentists. Being a Periodontist, my advanced training and skills are ideal for people who have any level of periodontal disease as well as those who want or need dental implants.
When it comes to dental implant patients, what I see most often are those who have worn dentures for a number of years who are exhausted with the uncomfortable rubbing and the inability to eat the foods they once enjoyed.
These patients typically tell me that their denture fit snugly when it was first made. Over time, however, they started noticing that the denture would cause sore spots on their gums. It would move when they chewed certain foods, even when they used denture adhesives or pastes.
I’ve heard patients describe how painful it is to have something as small as a strawberry seed or nut particle become trapped under the denture, piercing into their tender gum tissue. Some have shared how they had to eventually switch to a diet of soft foods that dissolved easily so they wouldn’t have to chew. And, many admit that they started declining invitations that included a meal.
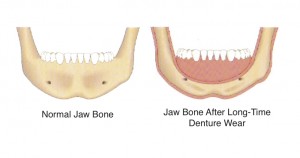
What many people don’t realize when they first opt for a denture is what occurs underneath the gum tissue. This is where the problem lies. It’s not that the denture is shrinking or changing shape. It’s your jaw bone. And the pressure placed on the bone from wearing dentures is only making matters worse.
When natural tooth roots are removed, the jaw bone that once held them is no longer fed the stimulants that kept it healthy. After a few years, it will shrink in height. This decline in mass is what causes changes in facial appearance, such as deep wrinkling around the mouth and the formation of jowls. And, it’s what causes the denture to move.
As time goes on, so does the process of bone loss. This means that the ‘ridge’ your denture was designed for flattens. A reline can rebuild the denture to accommodate some of the change. However, as the bone continues to decline, the denture continues to be ill-fitting.
While the pressure of wearing a denture certainly accelerates the rate of bone loss, a number of denture wearers also sleep in their denture. This round-the-clock pressure speeds up the rate of bone loss even more.
Not being able to eat and fear of embarrassment are common complaints of denture wearers. The solution is dental implants. Not only do implants restore the ability to bite and chew comfortably, they halt the bone loss associated with dentures. This is because they recreate the presence of tooth roots in the jaw bone.
When it comes to your smile, words like rocky, wobbly and slippery should never be a part of the description. When people opt for dental implants to replace an unstable denture, they smile, laugh, eat and even sneeze with confidence.
Eating a healthy diet, socializing with friends and family, and feeling confident are not luxuries. They are essential to a healthy, happy life. Call 828-274-9440 to schedule a consultation. During this, I’ll explain the type of implants that may be best for your needs and goals. We can also discuss estimated costs and payment options.
Important To Keep Your Dentist Updated On Your Medications
Posted on Mar 09, 2016 by William J. Claiborne, DDS MS
So what does the prescription you take for high blood pressure have to do with your dental care? And, why should you bother to tell us if you’re taking a supplement for anxiety?
Many medications don’t interact well with other medications, and even some supplements. It is important that your dentist and dental specialist have an up-to-date list of ALL medications you take. Here is why:
Medications such as Heparin or Warfarin help to reduce blood clotting, which lowers your risk for stroke and heart disease. That’s good. However, it is important that your dentist know about these since they can cause bleeding problems during oral surgery or periodontal treatment.
For those who take medications that help to strengthen bones, these have been associated with a rare but serious condition called osteo-necrosis of the jaw. Simply put, it refers to death of the bone. These prescriptions include Fosamax, Actonel, Atelvia, Didronel and Boniva and are taken to help prevent or treat osteoporosis. There are also versions administered by injection, including Boniva IV, Reclast and Prolia.
Osteo-necrosis of the jaw commonly occurs after dental procedures (tooth extraction, implant placement). Over 90 percent of those who have experienced osteo-necrosis are those who have taken the medication in repeated high doses due to cancer or other diseases. However, 10 percent who experienced osteo-necrosis were taking much lower doses, mostly intended to treat osteoporosis. Those who are taking these medications or have taken them within the past year should reveal this to their dentist.
Certain medications also affect the ability to taste, including cardiovascular agents, central nervous system stimulants, non-steroidal anti-inflammatory drugs, respiratory inhalants and nicotine skin patches.
Some medications can cause the development of oral sores, inflammation or discoloration of gum tissues in the mouth. These oral sores or discolorations may arise from taking medications for blood pressure, oral contraceptives and chemotherapy agents. Keeping your dentist aware that you are taking these drugs helps he or she monitor these areas closely and appropriately. Some spots and discolorations in the mouth can actually be symptoms of oral cancer. When your dentist is aware of the side effects of the medications you take, you can be adequately monitored without being treated for pseudo illnesses.
Dry mouth is a common side effect of a wide variety of medications, including those prescribed and over-the-counter. These include antihistamines, decongestants, painkillers, high blood pressure medications, muscle relaxants, drugs for urinary incontinence,
anti-depressants and many others. Drying causes the soft tissues in the mouth to become inflamed and makes you more susceptible to infection. When saliva flow is depleted, your risk for tooth decay and gum disease increases.
Supplements that may seem unconnected to your oral health can actually effect your care more than you realize. It is important for your dentist to know if you take…
• Ginkgo biloba or evening primrose – These herbs can reduce your blood’s ability to clot, possibly leading to excessive bleeding during and/or after a dental procedure.
• St. John’s Wort – This herb, which is often taken to reduce anxiety, can interfere with the metabolism of other medications, including sedatives, antibiotics and anti-inflammatory drugs such as prednisone and Decadron. When combined with St. John’s Wort, these drugs can be less effective. On the other hand, narcotics such as codeine, Vicodin and oxycodone can become more potent when taken with St. John’s Wort. This can lead to sleepiness, lethargy and dizziness.
• Valerian – This herb has mild sedative effects. If your dentist prescribes drugs for anxiety or painkillers containing codeine, the effects of both together are greatly accentuated. This can lead to severe sleepiness, lethargy and dizziness that can last into the next day.
• Calcium and magnesium – When these supplements are combined with certain antibiotics, they can decrease the antibiotics being properly absorbed. This can compromise your ability to fight off infection.
Your oral health is an important part of your overall health. Always keep your dental care givers updated on your health status and the medications (and supplements) you take.
Can You Reverse Gum Disease?
Posted on Mar 03, 2016 by William J. Claiborne, DDS MS
Our bodies are miraculous machines. They not only provide mobility and enable various functions, the human body is designed to heal itself.
When bacteria enter the body, white blood cells are the microscopic soldiers that surge in for battle. Their job is to attack the bacteria and destroy it. As with any battle, however, when the odds are in favor of the enemy, the ‘good guys’ don’t always win.
Bacteria reproduce very rapidly. When they become too much for your body’s defense mechanism to overcome, infection begins. Just as a cut or scrape on the skin can become infected, oral bacteria can cause infection in the mouth. This overload of bacteria can evolve into periodontal disease, which is an inflammation that attacks teeth, oral tissues and the bone structures that support teeth.
Gum disease is characterized by sore gums that bleed when brushing, persistent bad breath, gums that recede from teeth and turn red in color, and pus pockets that form on the gums at the base of some teeth. In latter stages, gum disease will cause teeth to loosen and eventually require removal.
Most gum disease occurs because people are often unaware that bleeding gums or gum recession is not normal. Insufficient brushing, failing to floss and missing 6-month dental cleanings can lead to a build-up of bacteria that forms, at first, plaque. This is a sticky film you feel on teeth. When plaque is not removed on a regular basis, it forms a cement-hard colony of oral bacteria, known as tartar or calculus.
As your mouth is enduring the repercussions of oral bacteria accumulation, gum tissues and tooth enamel are being eaten away by the bacteria. There is a point where only dental treatment can eliminate the bacterial onslaught, especially when it has penetrated below the gum line. However, with prompt attention and proper measures, you can halt and reverse the need for dental treatment and the progression of gum disease.
Gingivitis is the initial stage of gum disease. Your symptoms will probably include gums that are tender in spots and some bleeding when you brush. These are warning signs that signal an immediate need for attention.
Begin by twice daily brushing with a soft bristle tooth brush and use a fluoridated tooth paste. Brush for at least two minutes per time. Floss daily. Be sure not to pop the floss between teeth to avoid damaging the gums. Move the floss in a back-&-forth motion between teeth to ease it down so you can scrape the sides of each tooth.
You can remove a tremendous amount of oral bacteria by using a tongue scrapper daily. Or, brush your tongue with your tooth brush at the end of each brushing. This helps to dislodge bacteria that is embedded in the grooves of the tongue.
Drink lots of water during the day. This will aid saliva flow that is designed to move oral bacteria from your mouth on a consistent basis. Avoid foods and beverages that are drying to oral tissues. These include coffee, colas, alcohol and spicy foods. Also, try to minimize the amount of sugar and carbohydrates you consume. These foods energize the reproduction of oral bacteria.
If you smoke, consider using an oral rinse that will replenish the mouth with moisture. The chemicals in cigarette smoke are terribly drying to oral tissues. Some oral rinses are specifically designed for producing moisture. This is helpful since dryness provides oral bacteria with a favorable environment for reproduction.
When these steps are taken for initial levels of gingivitis, your gums should be less tender and bleeding should cease in a week or so. If you do not see improvement after 1-2 weeks of implementing these measures, see a Periodontal specialist as soon as possible. This dental specialist can determine the precise level of gum disease you are experiencing and provide appropriate treatment.
The key is to act sooner than later. Gum disease only worsens without treatment. In the U.S., it is the leading cause for adult tooth loss. Your natural teeth are precious and worth saving. With a healthy mouth, having your natural teeth all your life is a reasonable expectation.
The oral bacteria of gum disease is also harmful to your health in other ways, too. This bacteria has been known to trigger inflammatory reactions elsewhere in the body. It can contribute to heart disease, arthritis, diabetes, stroke, preterm babies and impotency.
Call 828-274-9440 if you have questions about your gums or if you are experiencing any symptoms associated with gum disease.
Research Closely Ties RA To Gum Disease
Posted on Feb 10, 2016 by William J. Claiborne, DDS MS
As a Periodontist, I treat all stages of periodontal (gum) disease. In early stages, the condition causes gums to bleed when brushing, bad breath and gum tenderness. As gum disease progresses, gums become red in color and pus pockets form at the base of teeth. Eventually, teeth loosen and may require removal. Gum disease, to no surprise, is the nation’s leading cause of adult tooth loss.
Over the years, research has found a correlation between the bacteria of periodontal disease and a number of serious health problems. Due to the inflammatory triggers associated with the oral bacteria of gum disease, it has been linked to heart disease, stroke, memory loss, preterm babies, diabetes and impotency.
For people who have rheumatoid arthritis (RA), the condition’s association with gum disease seems unlikely. Yet, research is showing a remarkably close connection.
It’s not only been determined that both gum disease and RA share a genetic likeness, their clinical makeup shows similar structures, primarily in pathogens. A pathogen is an agent in the body that causes disease or illness. The pathological processes that occurs in both gum disease and RA are almost identical.
While it is apparent that both conditions cause chronic inflammation in tissues that connect to bone, researchers have found that both diseases also have a similar inflammatory trigger. Also alike is the particular species of bacteria found in periodontally-diseased oral tissues and tissues that surround joints in those who suffer with RA.
RA is a debilitating disease that destroys joints. It is disabling and painful. In most cases, RA emerges gradually, often beginning with morning stiffness along with weak and aching muscles. Joint pain follows, with joints feeling sore and stiff. RA is typically found in the fingers, wrists, elbows, hips, knees, ankles, toes, shoulder and neck.
As inflammation from RA increases, joints become swollen with symptoms including fever, disfiguring of hands and feet, numbness and tingling. There is no cure for RA and lifelong treatment is required. Treatment may consist of medications, physical therapy, or even surgery.
Like RA, periodontal disease causes pain, swelling, and tenderness. As it worsens, the associatedinflammation can lead to destruction of the bone that supports teeth along with surrounding tissues.
In one study, a particular pathogen associated with periodontal disease was found to activate the same destructive process of rheumatoid arthritis. It has also been shown that, by treating periodontal disease in RA patients, RA symptoms often improve. This is likely due to the system’s reduced burden of oral inflammation.
What’s exciting about the findings of these research findings is how oral health correlates so closely to one’s overall health. Yet, it’s a bit scary at the same time. When you realize that the presence of gum disease can so greatly increase your risk for serious health conditions, it should send up alarms. However, even in this advanced age of modern medicine, nearly 75% of the U.S. adult population have some level of periodontal disease.
Help spread the word about the link between your oral health and a healthy body, especially to those you love. Emphasize the need for a thorough oral hygiene regimen at home as well as a commitment to 6-month dental check-ups and exams. If you have signs of gum disease (as mentioned above), seek treatment at your earliest convenience. Gum disease will only worsen and will require more treatment time and expense as it progresses.
Call 828-274-9440 to learn more.
Recent Posts
Categories
Archives
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- August 2014
- July 2014
- June 2014
- May 2014
- April 2014
- March 2014
- February 2014
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012